
I’ve been following CRISPR as a diagnostic tool since the first papers from Doudna/Zhang groups. CRISPR technology has been around a little longer (although just seven years or so) and has already enabled unimaginable scientific breakthroughs.There is also an ongoing patent battle based around who invented the tech (Doudna&Chapentier or Zhang) and there may well be a similar battle in the diagnostics space. Its application to diagnostics is being touted as a revolution in the field…but this remain to be proven.
History of CRISPR Dx field:
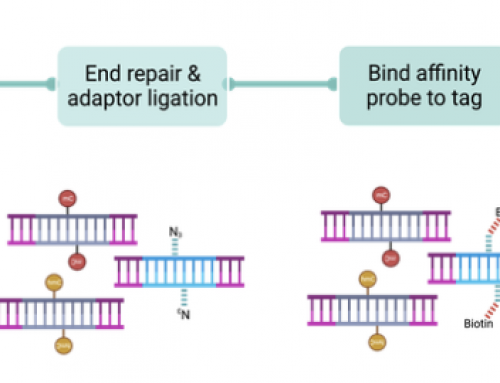
The major development in the use of CRISPR for diagnostics was the discovery of cutting activity on nucleic acids outside of the gRNA target site – when certain Cas variants bind to their target site they elicit “collateral cleavage” (East-Seletsky 2016) and degradation of ssRNA or ssDNA by Cas13 and Cas12a respectively. Addition of fluorescent reporters to the reaction enables detection of the variant of interest – on Cas/gRNA target binding a reporter signal is generated by cleavage of reporteds confirming presence of the target or mutation of interest. The Zhang lab used Cas13’s RNAse activity to develop Specific High Sensitivity Enzymatic Reporter UnLOCKING (SHERLOCK and SHERLOCKv2). While the Doudna lab uses DNAse activity of Cas12a’s to develop DNA Endonuclease Targeted CRISPR Trans Reporter (DETECTR).
Mammoth Biosciences: were first out of the gates in Summer 2018 with $23 million in Series A funding to develop DETECTR. Spun out of the Doudna lab by Trevor Martin, Janice Chen and Lucas Harrington Mammoth aims “to democratize disease detection with a credit-card sized, point-of-care test for fast, easy, and affordable detection of multiple conditions at once, for use both in the hospital and at home.” They demonstrated the effectiveness on HPV serotyping for types 16 (HPV16) and 18 (HPV18), which increase risk of HPV-related cancer, by analysis of patient samples using a crude DNA extraction and PCR amplification to enable a one hour test. The delivery of low-cost POC tests is likely to have hugely significant impacts in under-developed countries where testing is simply not performed because labs are in short supply or tests are too expensive. These guys aim to change the world (of testing)!
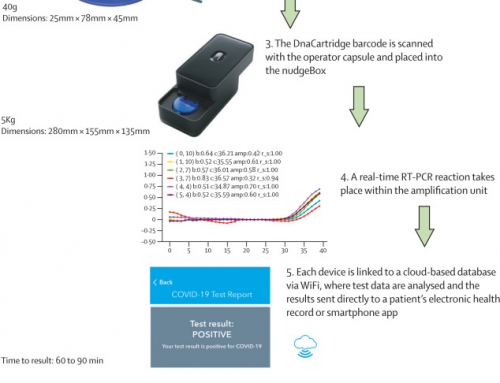
Sherlock Bio: announced $35 million funding to develop SHERLOCK and INSPECTR as “a molecular diagnostic answer for any sample, any target, anywhere.” Founded by Feng Zhang, Jonathan Gootenberg, and others to “disrupt diagnostics with better, faster, affordable tests”. In the SHERLOCKv2 paper Gootenberg et al showed how a combination of CRISPR enzymes could be multiplexed in four channels to enable sensitive detection. The multiplex test uses a visual readout on lateral flow strips in just 90 minutes. They reported results for ZIKA or DENV and a rapid genotyping assay after a 10 min DNA extraction from saliva with no additional purification in under 23 min (fluorescence) or 2 hours (lateral flow). The INSPECTR (Internal Splint-Pairing Expression Cassette Translation Reaction) technology has been licensed in from the Wyss Institute and uses synthetic gene networks as programmable molecular diagnostic devices. When the gene network detects a nucleic acid target, a bioluminescent reporter protein is produced that generate the signal for diagnostic readout delivering instrument-free, simple-to-operate diagnostic tests (based on lateral flow immunoassays).
Another method developed at the Shanghai Institutes for Biological Sciences uses the SHERLOCK method but substitutes Cas13 for Cas12 and RPA+IVT for PCR amplification. It delivers a “one-hour low-cost multipurpose highly efficient system”) for diagnostics: SHERLOCK HOLMES! The wit and inventiveness of scientists never ceases to amaze me!!!
Point-of-care lateral flow diagnostics:
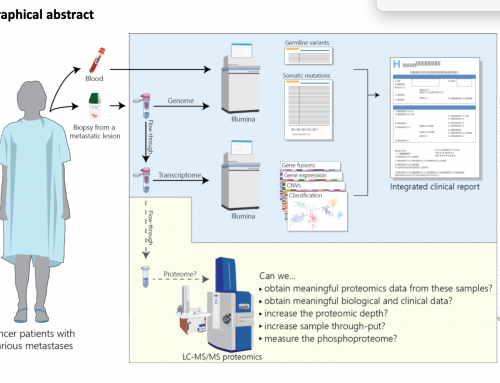
A major aim of both Mammoth and SherlockBio is to develop very low cost simple-to-operate diagnostics for easy deployment. This could be deployment to a hospital NICU, to a GP surgery, to a refugee camp in Syria or in your own home (maybe as DTC tests). Lateral flow assays (such as pregnancy tests) enable very simple testing and can be mass produced enabling low-cost. Ideally they can work directly from a biosample e.g. saliva in the case of germline genotyping. But for oncology diagnostics the field is going to need to work directly from plasma, or after ctDNA extraction and so will require a blood draw and minimal prep at the very least – this is likely to be done in a doctors surgery but in the longer term future could conceivably be done in Boots/Walgreens!
It’s very early days for CRISPR as a diagnostic tool and it looks like the battle lines are being drawn in much the same manner as before.





Leave A Comment