Can transplant genomics help better understand ctDNA?
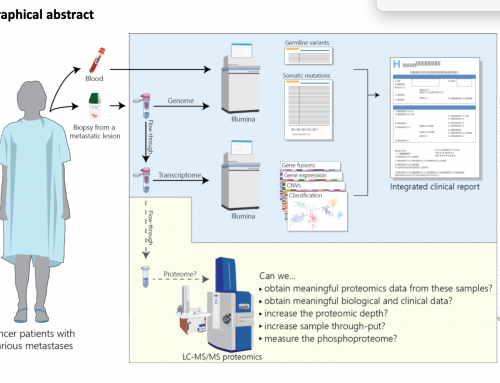
Circulating cell free (cfDNA) of tumour (ctDNA) is released by apoptotic and necrotic cells into blood and other bodily fluids. It has transformed NIPT and is transforming Cancer medicine. However the biology behind it’s release is still not wholly understood and this lack of understanding is likely to hinder our ability to develop novel methods and/or maximise detection sensitivity in clinical assays.
One difficulty that researchers face is that even in Cancer patients the differences between cfDNA (from normal cells, especially haematopoietic cells) and ctDNA (from tumour cells) is pretty minimal. Most of the genome is identical making it difficult to sort cfDNA from ctDNA. It is possible to enrich for tumour fragments by selecting DNA with a size range of 90-150bp; this can enrich for ctDNA up to 11 fold. But even then there are still only the somatic changes that vary between normal and tumour DNA making analysis a needle-in-a-haystack problem. And as researchers ideally want lots of ctDNA to work with there is generally never enough blood drawn from a patient to do all the testing a group might consider.
Transplant patients as a source of controlled cfDNA
What would help is to find a source of cfDNA that is somewhat inexhaustible and with a defined level of cfDNA. My suggestion would be to look at transplant patients. Each has an organ from another individual so the cfDNA from the transplanted organ is going to be clearly distinct from their own normal genome. With some 3-4 million SNPs between two individuals it would be possible to confirm the cfDNA that do not originate from the haematopoietic cells. Understanding how this cfDNA differs from organ to organ may shed light more on the mechanisms behind its release.
There are some 4-5000 organ transplants per year in the UK alone: 2000 Kidney, 1000 Liver, 200 Heart, 200 Lung and 200-300 others. With a small cohort from each organ it may be possible to discern organ-specific mechanisms of cfDNA release.
Organ donors are also pretty healthy so collecting blood might be as simple as taking a pint and separating it out the plasma into 300+ 1ml aliquots after centrifugation – that’s a good control sample. And that transplant patient may be able to keep giving year on year for a research project.
Transplant patients for ctDNA
Understanding the differences between cfDNA and ctDNA is the big challenge. Most cancer patients are not going to be bled to deliver the volumes of plasma that could be obtained from a healthy transplant patient, and they would have only a very small number of somatic variants separating their cfDNA from ctDNA.
But transplant patients may also get cancer of their transplanted organ – although it is unclear whether this likelihood is higher or lower than the normal rate (as reported on CRUKs cancer incidence statistics). Assuming the rate is the same as a non-transplanted organ them there are a small number of patients who have ctDNA that is truly distinct from their normal cfDNA: they represent a “transplant genomics” opportunity.
These unlucky people do represent an opportunity to better understand ctDNA and to develop better pre-analytical and analytical methods. With ctDNA already showing such promise their plasma may be important in pushing the limits of what we can do with ctDNA as far as possible.
With an estimated 125,000 organs transplanted globally, and with most of those patients being carefully monitored it should be possible to pick up the 10s or low 100s of patients who develop cancer. If done as a worldwide study then a “transplanted organ Cancer Genome Project” could allow us to ask if these cancers are distinct from the disease that arises in a patients own organ? If the Global Observatory on Donation and Transplantation do not record this information today it might be a good idea to start doing so.








Leave A Comment