Many of my followers in the cancer space, especially the Hemes folks, will already understand what MRD is and why it’s important. But for those of you who don’t know I thought an explainer might be helpful. I took inspiration from Keiths COVID qPCR explainer and this post is similarly intended for non-scientists who work in the NGS field e.g. financiers, reporters and the lay person. Apologies – there will be jargon I neglect to explain, it may get too technical and there may be inaccuracies (all of which I’d be happy to correct via the comments section). Here goes…
An introduction to MRD or Minimal Residual Disease:
Minimal Residual Disease or MRD is the term used to describe detectable signs of cancer in a patient who has had curative-intent treatment (usually surgery, radiotherapy, chemotherapy, immunotherapy, often in combination). It was initially used in haematological malignancies i.e. leukaemia’s and other cancers of the blood and lymphatic system. These “Heme” cancers are caused by a massive over-production of tumour cells, which crucially all carry a specific genetic mutation e.g. the chromosomal translocation BRC-ABL1 (the Philadelphia chromosome. The MRD test relies on its detection to indicate the presence of residual cancer cells in a patient. MRD positive patients often had worse prognosis, relapsed earlier and ultimately died earlier than patients who were MRD negative.
MRD tests were, and still are, based on the use of polymerase chain reaction (see Keiths PCR explainer) to amplify and detect the presence of the leukaemia-specific DNA sequence e.g BCR-ABL1 in a patients blood DNA; or flow-cytometry, where the cells themselves are analysed. It is a simple and very sensitive test but there is still room for development. The latest clonoSeq MRD test from Adaptive use NGS of the patients cancer to determine specific rearrangements to use for MRD detection, but the basic principle is the same as before.
Whichever MRD test is used it generally gives a simple positive or negative result. This enables a doctor to check if the patient has been “cured”, to monitor their response to therapy or status of remission, and assess different treatment regimens in clinical trials of new drugs via a simple test rather than relying on imaging of the cancer in a CT scanner, which is usually less sensitive and requires a visit to a specialist clinic.
The figure below is from a brilliant piece written by Nancy Valente, MD (VP Hematology/Oncology, Genentech/Roche).

Fig 1: MRD development over the last 30 years
Novel developments in MRD for solid tumours:
As already stated above MRD is part of standard clinical practice for blood cancers. The use of MRD in solid-tumours e.g. Breast, Lung, Prostate is much newer but several recent advances give a glimpse into the future for solid cancers where MRD is likely to be standard-of-care in just a few years time (see References). Early reports on the correlation of the levels of DNA released into the blood by tumours (circulating tumour DNA or ctDNA) after surgery and outcomes showed that patients with high-levels of ctDNA did badly compared to those with low levels (Figure 2). The explanation for this is that high ctDNA burden indicates the presence of tumour; either remaining at the site of surgery or in the form of distant metastases, that will come back sooner in those patients. Detection of this ctDNA should enable more aggressive treatment of these patients or treatment ahead of recurrence as detected by imaging i.e. earlier that current SOC to improve outcomes.

Fig 2: Four of the major papers reporting MRD detection for solid tumours using ctDNA (see references for links to these papers)
Challenges in solid tumour MRD:
Solid tumour MRD tests are harder primarily because of two reasons 1) most solid cancers are unique to the patient and only carry very small numbers of, if any, genetic mutations that are the same in every patien, which means designing a test is harder than in Leukaemias. And 2) solid tumours “leak” only a small amount of DNA, usually under 1%, into the blood as ctDNA meaning a much higher sensitivity test is required than for leukaemias where a large proportion of the blood DNA may be affected.
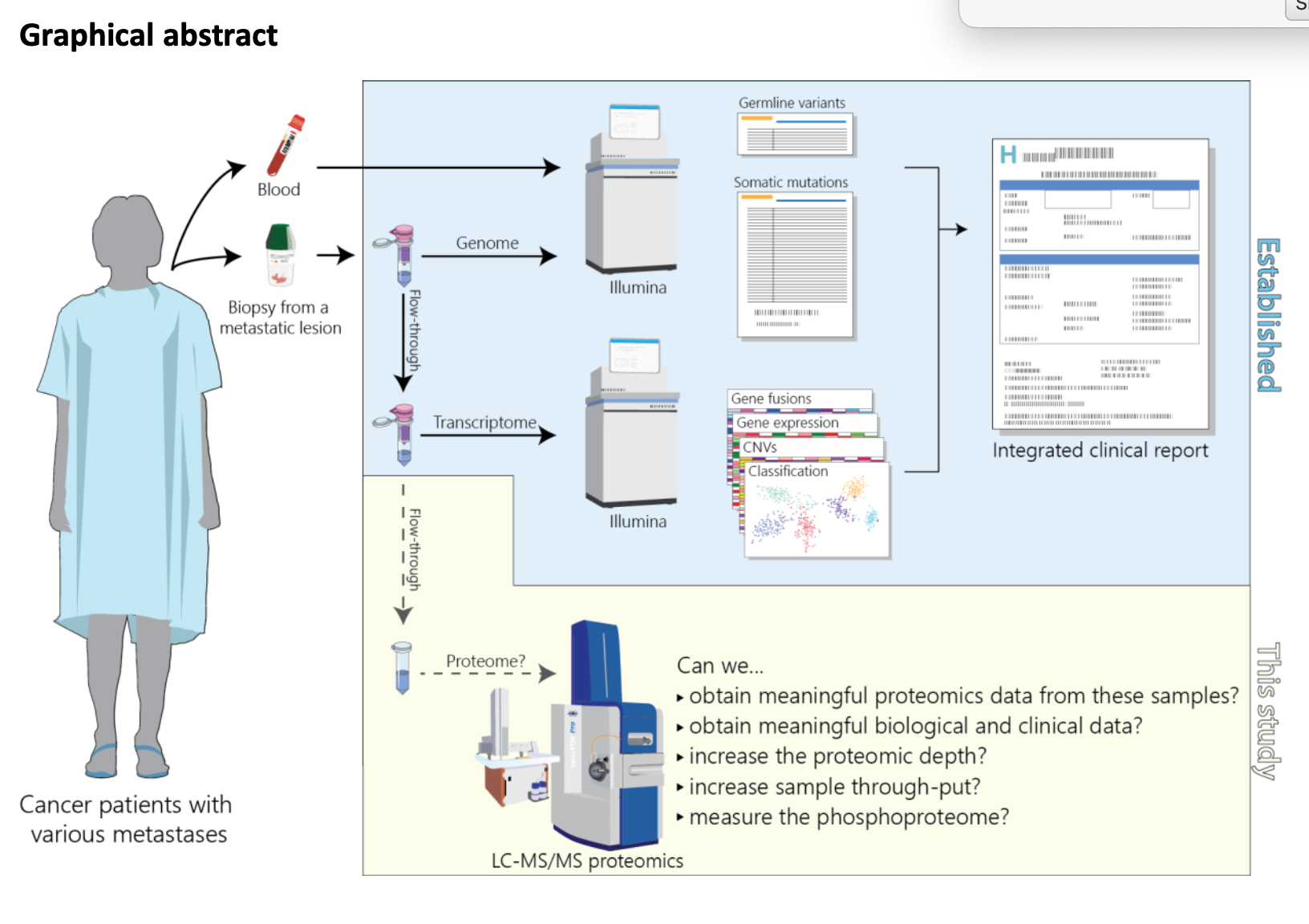
The uniqueness of cancer in patients means that the MRD tests currently being developed are personalised assays. This means that each test is also unique and is designed to detect the mutations in that single patients tumour. Several companies are developing MRD assays: Natera, ArcherDx, Genosity, Inivata; to do this they all use a similar workflow, which begins with generating DNA sequence data (usually Whole Exome Sequencing) from the patients tumour, to identify somatic variants (mutations only found in the tumour), and blood, to remove CHIP variants (mutations only found in the blood), that will ultimately make it into the test. Around 10-50 variants (usually truncal mutations i.e. found in most of the cancer cells) are taken forwards into the MRD assay development for primer/probe design. These primers/probes are used in either a PCR assay or a hybridisation-capture assay as the basis of the MRD test that is usually performed about four weeks after surgery.
An approach by C2i Genomics uses Whole Genome Sequencing of the tumour to identify somatic variants that are then detected in Shallow Whole Genome Sequencing of blood. This uses the same up-front analysis of the tumour but the MRD assay does not need to be personalised, which may make it easier to roll out in the clinic.
Ultimately the success of MRD tests will rely on three things.
- Firstly, their sensitivity – the most sensitive assays should be able to detect ctDNA in all patients who need aggressive treatment as well as identify those patients who can be safely spared the additional rounds of surgery, chemo or radiotherapy.
- Secondly, they should be fast and easy to use – this may require moving to non-personalised and/or tumour-agnostic assays but could be solved by building MRD factories that develop the specialist workflows to be as slick as possible.
- Thirdly, they must be cost effective – this does not mean cheap, but it does mean the assay needs to save health care providers or insurers money over standard of care while improving patient outcomes.
Technological progress continues to push on all three fronts!
What’s next – epigenetic MRD?:
The opportunities for patients that come from MRD assays, enabling more aggressive therapy in some, or reducing the need for chemo/radio for others, means it is an area of rapid technological development right now. This is focused on the challenges one and two above, increasing sensitivity as well as building the MRD factories and/or developing non-personalised assays to make them easy and fast.
Although the technological progress is moving very quickly on creating personalised MRD tests the challenges of producing these bespoke assays are not being ignored. Many researchers are developing methods that are “patient agnostic” and can be run across any patient; some are also looking to develop “tumour agnostic” tests that could be run on any cancer in any patient – the ultimate goal.
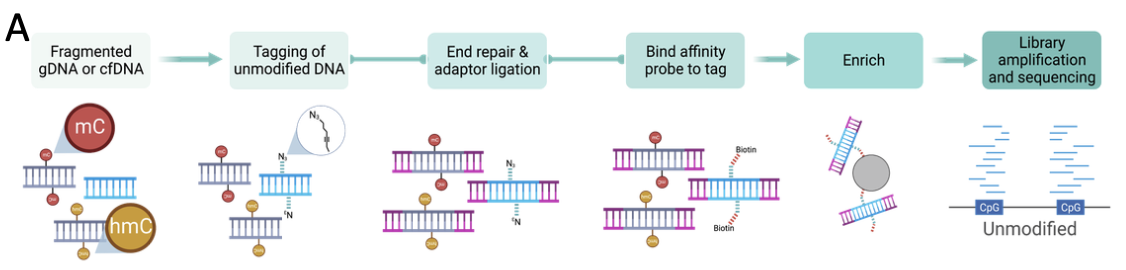
These agnostic methods use different epigenetic methods to detect cancer. These epigenetic assays detect changes in how the DNA of the tumour is marked chemically, or packaged in the nucleus, rather than focus on mutations in the tumour genome. These Epigenome “marks” more similar across different patients, and even across different cancers, and there are many more epigenetic changes than mutations in tumours, making them great candidates for new MRD tests. One company pushing hard on this frontier is GRAIL (recently acquired by Illumina) and slide 11 of their Transforming Cancer Detection presentation highlights what they are doing over the next few years with respect to MRD. GRAIL have developed a DNA methylation assay for cancer early detection, which relies on finding regions in the tumour genome that are methylated to detect the presence of cancer. Application of their technology, or something similar, to MRD might just lead to a single MRD test for any cancer.
The use of MRD in solid tumours is still in its infancy. But the impact on patients will likely be so positive that the research and biotech communities are investing heavily and are likely to make rapid progress. Roll on the next decade – the decade of MRD?






Leave A Comment